When you want to launch a health tech product, you need to be mindful of the compliance requirements that apply. Most healthcare providers are subjected to a set of complex, fast-evolving medical regulations. It’s not easy to comply with all laws, but yet, you must.
Such laws or guidelines are in place to ensure patient safety, data security, and interoperability amongst healthcare systems. In 2024, 92% of healthcare organizations reported at least a data breach. Such incidents can undermine the healthcare experience, which existing and new healthcare laws aim to safeguard.
I’m Yan Likarenko – Product Manager at Uptech. Over the years, I’ve helped healthcare startups and SMBs worldwide navigate the complexities of complying with global, regional, and local regulations.
I hope I can help you avoid such outcomes by providing a list of healthcare compliance examples, their purpose, jurisdiction, and to whom they’re applied.
Let’s start.
What is healthcare compliance? And who regulates it?
Healthcare compliance is the act of aligning healthcare practices to laws, regulations, and guidelines that govern medical establishments in certain regions. These laws exist to protect patients' rights and ensure medical practitioners operate in a safe environment. Often, healthcare compliance involves streamlining procedures across broad disciplines, including medical intervention, data security, medical coding, billing, and other areas.
Over the decades, new healthcare acts have been introduced to better regulate the industry as patient needs, technologies, and medical services evolve. I highlight several major laws that are pivotal in shaping the US healthcare industry.
- Health Insurance Portability and Accountability Act (HIPAA) was introduced in 1996 to regulate how medical providers collect, store, and protect patient’s data.
- The Health Information Technology for Economic and Clinical Health (HITECH) Act came into law in 2009, augmenting HIPAA to improve data security and promote the use of electronic medical records (EMR).
- The Affordable Care Act, 2010 requires healthcare providers to prioritize service quality and patient care experience and submit performance reports.
- No Surprises Act was enacted in 2020 as an effort to promote transparency in billing and prevent patients from receiving unexpected balance bills.
Many healthcare companies find it challenging to comply with various medical acts, mainly because the rules are complicated, extensive, and everchanging. Moreover, regulators might introduce stiffer penalties to ensure stricter adherence amongst organizations. For example, HIPAA recently increased the fines for non-compliance and introduced new policies to scrutinize anticompetitive practices.
Like all regulations, healthcare compliance is only effective if they are properly enforced.
- In the US, the Office of Civil Rights, Drug Enforcement Administration (DEA), and Food and Drug Administration (FDA) are among the key authorities in enforcing healthcare laws.
- In Europe, healthcare organizations are governed by laws set by authority bodies like the European Medicines Agency, National Competent Authorities, and the European Centre for Disease Prevention and Control.
- In Asia, healthcare laws are enacted by individual countries. For example, both the National Medical Products Administration and the Pharmaceuticals and Medical Devices Agency review and approve medical devices in China and Japan, respectively.
Healthcare Compliance Regulations Examples
If you’re starting a new healthcare business or expanding existing ones, compliance is a top priority. Specifically, if your company provides medtech apps, portals, or other solutions, you’ll need to be mindful of the following healthcare compliance examples.
Social Security Act
The Social Security Act is one of the earliest compliance regulations that regulate medical facilities in the US. The act ensures US citizens are granted access to basic healthcare necessities through programs like Medicare and Medicaid.
Health Insurance Portability and Accountability Act (HIPAA)
Since enacted in 1996, HIPAA has set the standard for healthcare data security in the US. HIPAA requires healthcare organizations to implement measures that keep patient’s information secure. Another role this act undertakes is ensuring US citizens enjoy gapless insurance protection in between employment. In short, patients are granted greater rights to healthcare and privacy with HIPAA.
Now, HIPAA remains one of the most important regulations that service providers must comply with, especially if they are developing healthcare digital products.
To explore specific areas that the act applies to, check out our HIPAA checklist.

Health Information Technology for Economic and Clinical Health (HITECH) Act
The HITECH Act strengthens HIPAA’s implementation further and also encourages healthcare organizations to adopt EHR in their medical workflow. Under the act, organizations must report a data breach impacting more than 500 individuals within 60 days. Or they might face penalties. And from our experience working with healthcare clients, the act also sets forth how organizations can implement EHR in a meaningful way.

False Claims Act
The False Claims Act should be taken seriously by healthcare providers operating in the US, given that civil and criminal penalties are involved. The same goes if you want to release a healthcare product for US citizens and medical professionals. The law forbids medical facilities from filing false claims or misrepresenting those services to receive a higher payout from the government. We don’t want to sound intimidating, but you should know that Precision Lens was fined $487 million for breaching a couple of laws, including this.

Anti-Kickback Statute
Since 1972, the Anti-Kickback Statute, or AKS, has been aggressively enforced to eliminate any potential inducement, monetary or otherwise, for referral . Hospitals, clinics and doctors cannot offer cash, discounts, gifts or anything to attract patients. Some healthcare providers found out the hard way that going against this law can be very costly. DaVita, for example, paid $400 million for violations they’ve committed.

Patient Protection and Affordable Care Act
The Patient Protection and Affordable Care Act, also known as Obamacare, gives Americans easier access to insurance, Besides, it makes healthcare more affordable. Insurance companies, for example, can no longer deny coverage or raise premiums based on pre-existing conditions.

Stark Law
Stark Law is one of the healthcare compliance examples that prevent conflicts of interest between medical experts and patients. The law prohibits self-referrals, which means that physicians cannot refer their patients to the medical establishments in which they have a financial interest. You’ve got to be specifically careful with this law because we’ve seen many healthcare companies get fined for violations. A recent case involves Erlanger, which allegedly overpaid their physicians and is seeking reimbursement from Medicare.

GDPR (General Data Protection Regulation) (EU)
The GDPR is one of the most important data privacy laws that healthcare providers in the region must follow.
Essentially, the regulation provides patients with the right to know and control how their data are processed. Furthermore, patients can ask healthcare providers to correct or remove their data from the database. In addition to protecting patient’s privacy, healthcare organizations must also notify the Information Commissioner’s Office within 72 hours of a data breach.
When building an app, we suggest working with a development team familiar with data security measures. For example, our team has built apps that target the EU market and require strict compliance with GPDR.

21st Century Cures Act
One of the modern healthcare regulations, the 21st Century Cures Act provides various measures to speed up medical research and development. Also, under the act, medical facilities must ensure patients can easily access their medical records. They do so by allowing the inter-exchange of EMRs amongst disparate healthcare systems.

CCPA (California Consumer Privacy Act
The CCPA is a state-specific data privacy law that regulates organizations serving Californian residents. Healthcare organizations must comply with the law if they operate in California.
According to the act, patients have the right to know how their data are collected, stored, and managed, which seems quite similar to HIPAA. However, CCPA’s scope extends beyond medical information, which means healthcare providers must provide adequate data security measures for non-medical information they collect.

Interoperability and Patient Access Final Rule
The Centers for Medicare & Medicaid Services introduced this act to streamline healthcare services. Basically, the act encourages medical providers to share information with other parties through an application programming interface. So, if you want to comply with this act, you’ll need to work with developers familiar with API. Our team, with experience building and integrating software components, is one.

Medicare Access and CHIP Reauthorization Act (MACRA)
MACRA mostly changes the decades-old Medicare Act. It also included the establishment of the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs) programs. These align with NOHS principles which keep providers paid for quality care over quantity served. The act requires healthcare providers to establish such a restructured payment model in their individual systems.

No Surprises Act
As the name implies, the No Surprises Act is a legal measure that protects patients from bills that were charged without their knowledge. For example, patients might be treated by facilities in out-of-network facilities, which incurs charges unbeknownst to them. With the No Surprises Act in place, there are limits to how much patients can be billed.

Emergency Medical Treatment and Labor Act (EMTALA)
EMTALA is another key regulation that grants US citizens access to basic healthcare. This act, in particular, ensures all patients, regardless of their ability to pay, have access to medical screening when they present themselves in emergency departments. The act also prohibits patient dumping, an incident where uninsured or underinsured patients are transferred from private to public facilities without being granted the necessary medical care.

What Are the Penalties for Non-Compliance?
We know that Community Health Network Inc. paid $345 million in 2023 for breaching Stark Law. But are legal penalties the only worry you have for breaching healthcare acts? Below, we share the consequences that healthcare will bear if they don’t take compliance seriously.

Monetary fines
Authorities can impose hefty penalties on medical organizations, as stipulated by the law. For example, you could be fined up to $71,162 per offense if you fail to adhere to certain HIPAA regulations. Meanwhile, violators of GDRR, which is enforced in EU, can face up to €20 million fine or 4% of a company’s global annual revenue from the previous year, whichever is higher.
It’s important to realize that these aren’t empty threats, but instead, penalties that have been diligently enforced. Many organizations have paid the price for oversights, whether intentionally or not, in their compliance efforts. One of the latest incidents involves Cerebral, Inc, a telehealth company. The FTC found the firm guilty of sharing personal health information in its advertising campaign, which led to a $7 million fine.
Legal implications
Some healthcare regulations might impose criminal charges on key stakeholders when found guilty of breaching the acts. For example, violating the Anti Kickback Statute can land the perpetrator up to 10 years in prison or $100,000 in monetary penalty. Even if organizations are spared from criminal prosecution, they may end up with civil lawsuits, which can cost them significantly. Just take the Halifax case, where the hospital paid $85 million in settlements for violating Stark Law.
License revocation
On top of monetary penalties, medical establishments may also have their license revoked for failing to comply with stipulated acts. If this happens, they can no longer continue providing medical services and patient care like they used to.
Reputational losses
Although not a direct penalty, healthcare organizations may suffer reputational damage, which some find hard to recover from. When patients lose trust in a brand, the consequences can be just as significant — If not more severe — than monetary fines. Medical organizations might suffer financially as patients turn to their competitors.

How to Maintain Healthcare Compliance in Your Software? 7 Steps
I’ve shown you examples of healthcare compliance, and the risk of not adhering to laws. Whether you want to scale a digital product or plan to build one from scratch, make compliance a priority from the start. Otherwise, you’ll find it more difficult to make changes when you’ve onboarded more patients, doctors, insurers, and other medical stakeholders.
Let’s say you’ve launched a healthcare app that doesn’t comply with HIPAA and has been using it for years. You’ll have a tough time rebuilding the entire data pipeline, which can disrupt daily workflows. Plus, depending on the complexity, the modification might take a long time to complete. And that could impact your organization’s financial standing.
At Uptech, we’ve worked with healthcare startups and SMBs, such as this mental healthcare app that serves the US market. So, we know the challenges and what to pay attention to if you want to comply with healthcare regulations, particularly in the US.
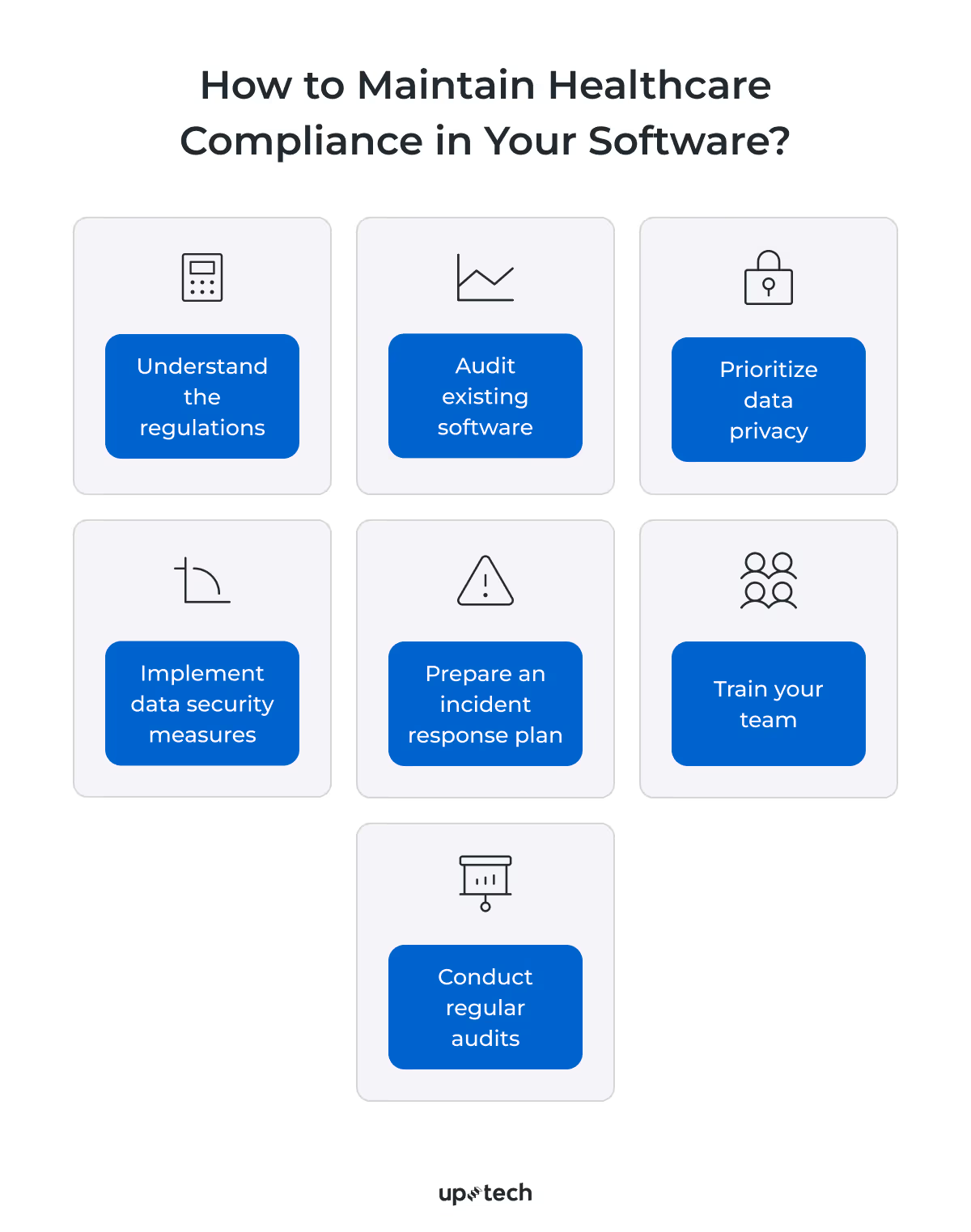
Step 1. Understand the regulations
Learn what are the requirements your software needs to comply with. For example, if you build a healthcare CRM, the typical acts that apply are HIPAA, HITECH, and CCPA. Make sure your team learns specific terms, policies, scope, and consequences of non-compliance.
As a precaution, run through the list of examples of healthcare compliance we share again and go through the official documents.
Step 2. Audit existing software
If you already deploy healthcare apps, ensure all services used in your app comply with relevant regulations (e.g., HIPAA). You can do it by conducting a thorough risk assessment — ideally through a qualified third-party auditor who can grant official certification.
Pay attention to potential software and database vulnerabilities that could be exploited by cybercriminals or lead to accidental data breaches. Also, map and analyze the entire patient care workflow to confirm that every process aligns with the required compliance guidelines.
At Uptech, we work with these compliance requirements every time we build products that collect personal data, so we know all the nuances inside and out. While we don’t provide the official audit or certification ourselves, we guide you using our compliance checklist, working with compliant 3rd party vendors only, and ensuring your product meets all necessary standards. This way, your application can confidently be called fully compliant.
Step 3. Prioritize data privacy
When you build healthcare software, you’ll need to collect health information. But before you do that, make sure patients are aware of what is being collected and how it will be used. For example, you can make data privacy policies more visible on the app.
On top of that, the developers you work with can limit the type of information collected. At Uptech, we only store information that your apps need to function. And even that, we try to aggregate or anonymize sensitive health information to protect the patient’s privacy.
Step 4. Implement data security measures
On paper, securing healthcare data looks simple, but in reality, most healthcare practitioners need help because of the complex environment in which health tech apps operate. For example, a clinic needs to ensure that the patient portal, physician administration software, mobile app, and backend infrastructure are aptly protected from unauthorized access.
Most countries have strict laws that penalize healthcare establishments that don’t take data security seriously. So, if you haven’t yet, start applying measures like encryption, multi-factor authentication, and role-based access to regulate data collection, storage, and usage.
If you struggle to keep healthcare data safe, reach out to our team. Uptech has a solid track record of building secure apps that comply with stringent data privacy regulations, including HIPAA and GDPR.
Step 5. Prepare an incident response plan
Despite your best efforts, mishaps may happen. In such cases, you’ll need to promptly react to prevent data loss and keep the facility operational. And this means putting disaster recovery options in place, such as data backups and other fail-safe measures. Also, your team needs a clear chain of action the moment your software is breached.
Step 6. Train your team
Healthcare compliance is a team effort. The responsibility doesn’t fall on app developers alone. All stakeholders, including doctors, nurses, medical staff, and administrative personnel play an equal role in adhering to data privacy and healthcare laws. Therefore, conduct training to ensure they fully understand the rules that govern your app.
Step 7. Conduct regular audits
Healthcare regulations may change from time to time to meet ongoing requirements. To remain compliant, continuously assess your software and make appropriate changes.
When Healthcare Compliance Meets AI: How to mix these two?
There’s no doubt that AI will improve the patient care experience, but without proper measures, you will face challenges in adhering to healthcare compliance regulations. Below, I share ways to integrate AI with healthcare without compromising data security, patient trust, and legal requirements.

Tip 1: Ensure transparency in the development of AI systems in healthcare
Be upfront if you want to use AI in existing or new healthcare software. Both medical professionals and patients have the right to know how AI affects them. To foster transparency, document the type of AI models used, conduct testing.
Plus, it’s also helpful to establish a framework that helps stakeholders understand the benefits and risks that AI brings. With the framework, stakeholders can justify investing in AI and make informed decisions where patients’ well-being is concerned.
Tip 2: Address biases in AI algorithms
AI models can sometimes produce biased results, which might affect decisions made throughout a patient’s care journey. To reduce such cases, ensure that the data samples are diverse and fairly represent the patients’ demographic.
We also recommend a human-in-the-loop approach, where critical decisions are reviewed by a medical professional before they’re acted on. Let’s take clinics that want to use chatbots in healthcare as an example. Instead of automatically replying to all patients’ queries, we can help you to filter and route those that require human intervention to trained medical experts.
Tip 3: Validate the output generated by AI to ensure the accuracy and credibility of information
Although AI models have shown remarkable improvement, they might sometimes hallucinate or produce inaccurate output. During testing, it’s important to validate the model’s output. Pay attention to misleading information, irrelevant results or biased output, which can negatively affect the healthcare system.
Tip 4: Prioritize privacy with robust measures to protect users’ data
AI, or specifically generative AI in healthcare, involves collecting, storing, and processing massive protected health data. And that makes healthcare organizations a likely target by cybercriminals. So, it makes sense to secure the data pipelines, whether by encryption or other protectionary measures.
Tip 5: Ensure ongoing maintenance of AI algorithms for performance, accuracy, and reliability
The AI models you use may become inconsistent over time. Or they might be obsolete because of changing requirements and trends. As the service provider, you’ll need to constantly test, and make changes to ensure the AI algorithms continuously meet the desired performance standards.
Tip 6: Establish clear lines of accountability for the development, deployment, and outcomes of AI systems in the healthcare system
Ultimately, each individual must answer for decisions they make, even with AI in the picture. It’s unethical to pin the blame on AI when things go wrong in patient care. So, healthcare providers should understand how AI systems are trained and engage developers experienced in building reliable AI-powered software.
On top of that, it’s prudent to put human checks in place, particularly when making critical decisions. Remember, AI isn’t meant to replace medical professionals but acts as a guide to simplify their job.
Tip 7: Form an ethics committee or engage a review person for the ethical oversight of the output
Healthcare founders and CTOs may need help ensuring the AI system they develop adheres to ethical principles. An ethics committee keeps the development in check by reviewing AI technologies and advising your team if they find possible ethical risks.
FAQ
What is healthcare compliance?
Healthcare compliance describes measures that medical establishments take to obey laws, regulations, and guidelines in specific regions. For example, hospitals and clinics in the US must comply with HIPAA, HITECH, False Claims Act, and other healthcare compliance regulations.
Why is compliance important in healthcare?
Medtech startups and small businesses strive to improve patient care delivery, build trust, and ensure a safe medical workspace. Healthcare compliance helps them in achieving those goals. On top of that, strict adherence to health acts steers organizations away from monetary penalties and legal cases.
How to check for healthcare compliance?
The best way to do so is to identify the laws you need to comply with. Then, run an internal audit on your existing software and workflows. From there, identify security gaps and areas of non-compliance that might compromise data security, patient privacy, and safety.
Who is responsible for compliance within a healthcare organization?
Usually, the compliance officer takes charge of compliance efforts in a healthcare establishment. That said, the Office of the Inspector General (OIG) recommended these key roles to create an effective compliance program.
- Chief Compliance Officer
- Compliance Team
- Health Information Management (HIM) Department
- Legal Department
- Quality Improvement Department
- Risk Management Department
- Clinical & Administrative Departments
- Board of Directors
- Providers, Clinicians, and Staff Members























































































.avif)









